Supporting Informal Healthcare Teams at Home using Sensor Data
Background: This project is a major part of my dissertation research. Through this project I have gained a deeper understanding of how neurological impairements affect people and their families' life and I have found opportunities to use my skills to support them.
I joined the project initially to assist a senior Ph.D. student, Ayşe Büyüktür, with a qualitative study and data analysis, under the mentorship of two faculty advisors. Since then, I have taken the lead to focus particularly with respect to using my background in computer science to explore interactive system design.
My role(s): Project Leader, Researcher, Designer, Developer
Collaborator(s): Dr. Mark S. Ackerman, Dr. Ayşe Büyüktür, Dr. Michelle Meade, Dr. Mark W. Newman
Motivation: Teenagers with a chronic health conditions, such as spinal cord injuries deal with enormous challenges, including managing ever-changing health status, working with their care-teams in their everyday lives, maintaining their self-image, and coping with social expectation for them to be independent in the process of transitioning to adulthood.
Problem Solving: To provide important observations of the care experience, my team and I conducted interviews with 27 stakeholders to understand how sensor-based technology can support care-team collaboration. As stakeholders might be new to sensors and data, I further conducted co-design activities with 1 patient so that insights could be drawn from sharing our knowledge and experience in continuous engagement.
I developed a system, Data Checkers, that enables users to visually compose sharing settings for fine-grained control and have evaluated it with 15 patients and caregivers through a comparison study.
I am currently developing and evaluating interactive systems to provide concrete examples that embody the lessons learned from the study.
Interview & Focus Group
27 stakeholders
Co-design
1 patient
Protootype & Evaluations
15 participants
Card Sorting
24 participants
Interviews
30 participants
Outcomes:
Findings:
- Independence is achieved collaboratively: a patient's independence is achieved through collaboration since the distribution of responsibilities directly affects the quality of independence.
- Responsibility is continuously redistributed: the distribution of responsibilities changes based on the patient's health and the stability of different care routines.
Major design suggestions:
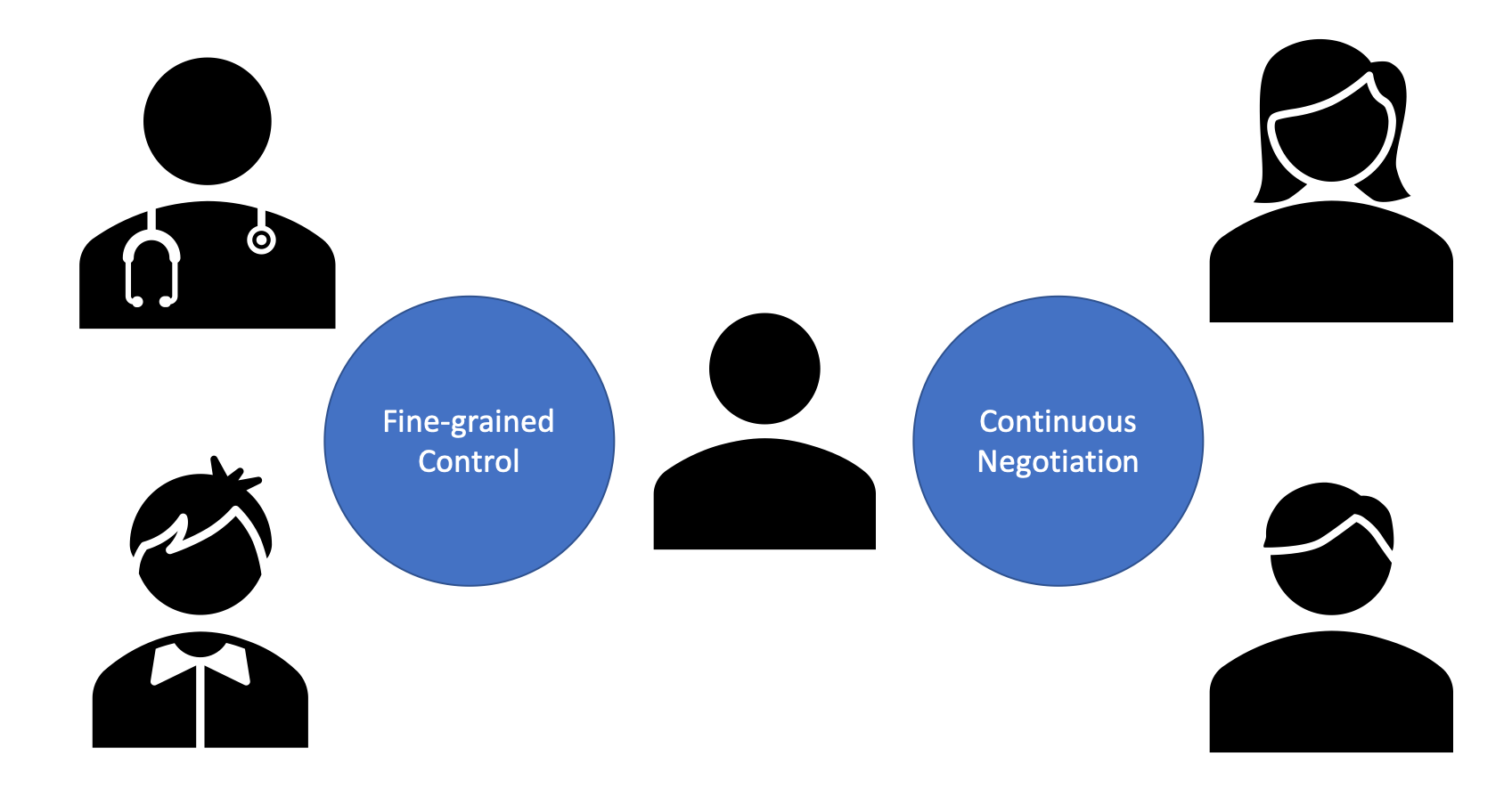
- Support fine-grained control to enable a sense of independence: sensor-based technology should allow data sharing to be continuously negotiated with fine-grained control among a patient, family, paid caregivers, and clinicians to accommodate the patient's desired level of independence.
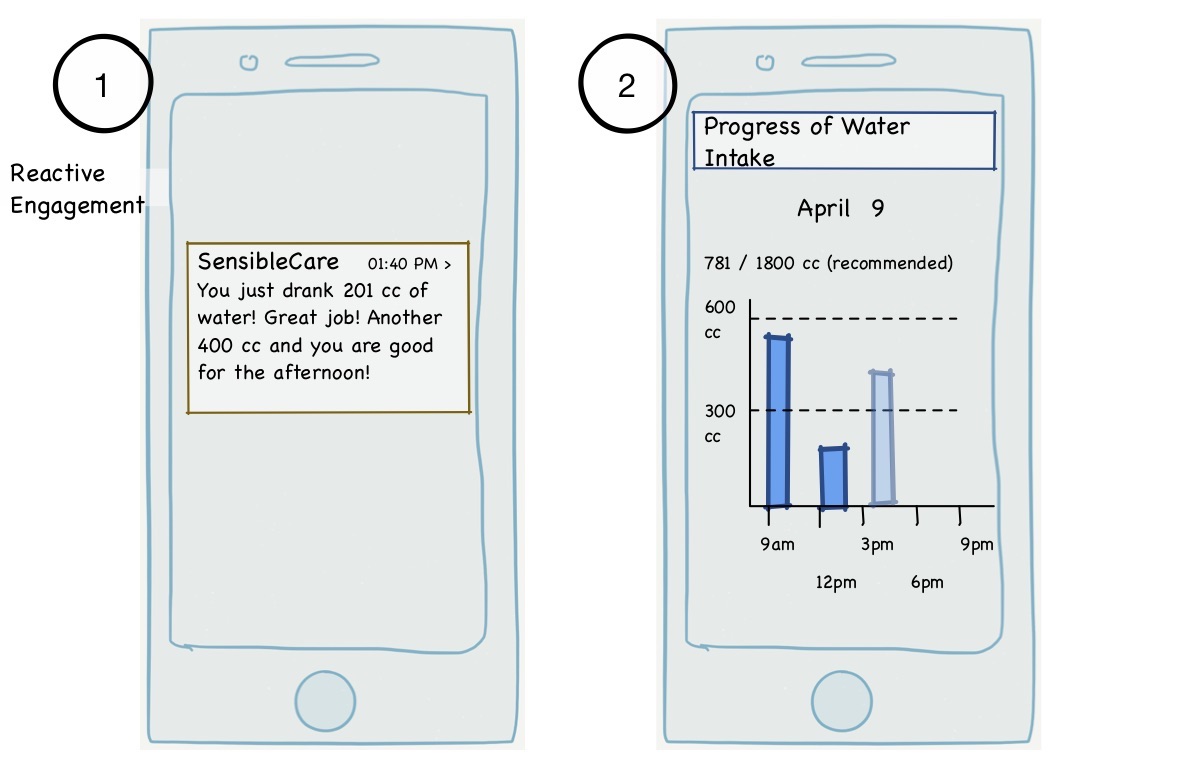
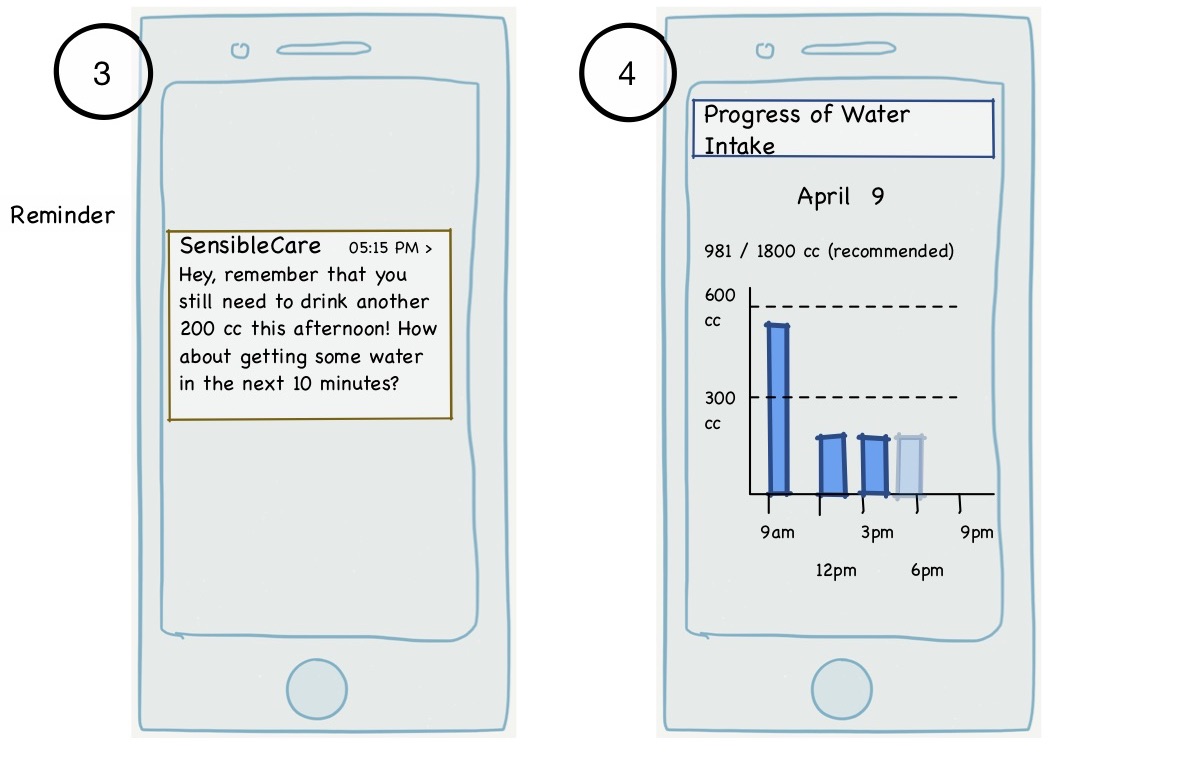
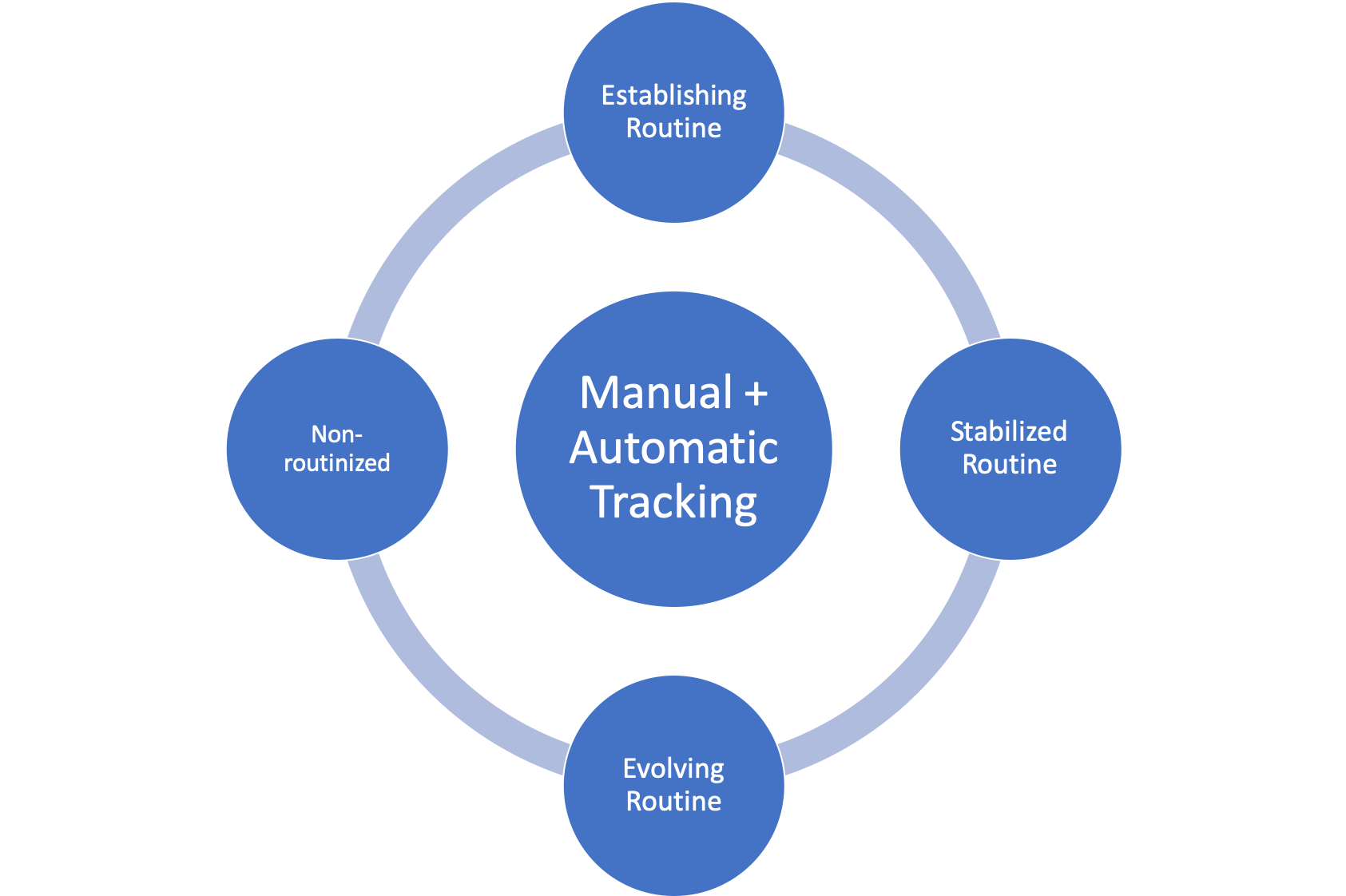
- Tailor system proactiveness to provide an appropriate level of engagemnet: sensor-based technology should tailor user engagement with different levels of proactiveness to align with the stability of care routines.
I am still continuing the design and evaluation of Data Checkers. Initial analysis shows that participants can use the visual composition environment provided by Data Checkers to create and adjust sharing settings efficiently and flexibly. I have recently conducted two additional studies, and I am currently writing reports to summarize my findings on how to further simplify the process of creating sharing settings and using additional support to manage sharing through team collaboration.
The outcomes of this project include several scholarly publications (link) and a web-based prototype that allows patients to create sharing settings through a grid-based user interface.
Summary:
Date: 2017 ~ Present.
Research & Design Strategy
Understand Care Team Members' Lived Experience using Interview and Focus Group
The goal of the research project is to understand the lived experience of patients with neurological impairments such as spinal cord injuries and that of their family members, and clinicians, as such chronic care often time requires assistance from them. I am particularly interested in how members of such care team collaborate and coordinate with each other with the goal of informing the design of sensor-based technology that can collect data to support such collaboration.
The overall approach for this project is to ground our design based on a solid understanding of care teams' experiences. I employed multiple methods to understand the care team members' perspectives and invited a patient to co-design with the research team.
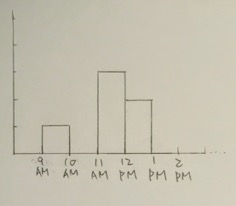
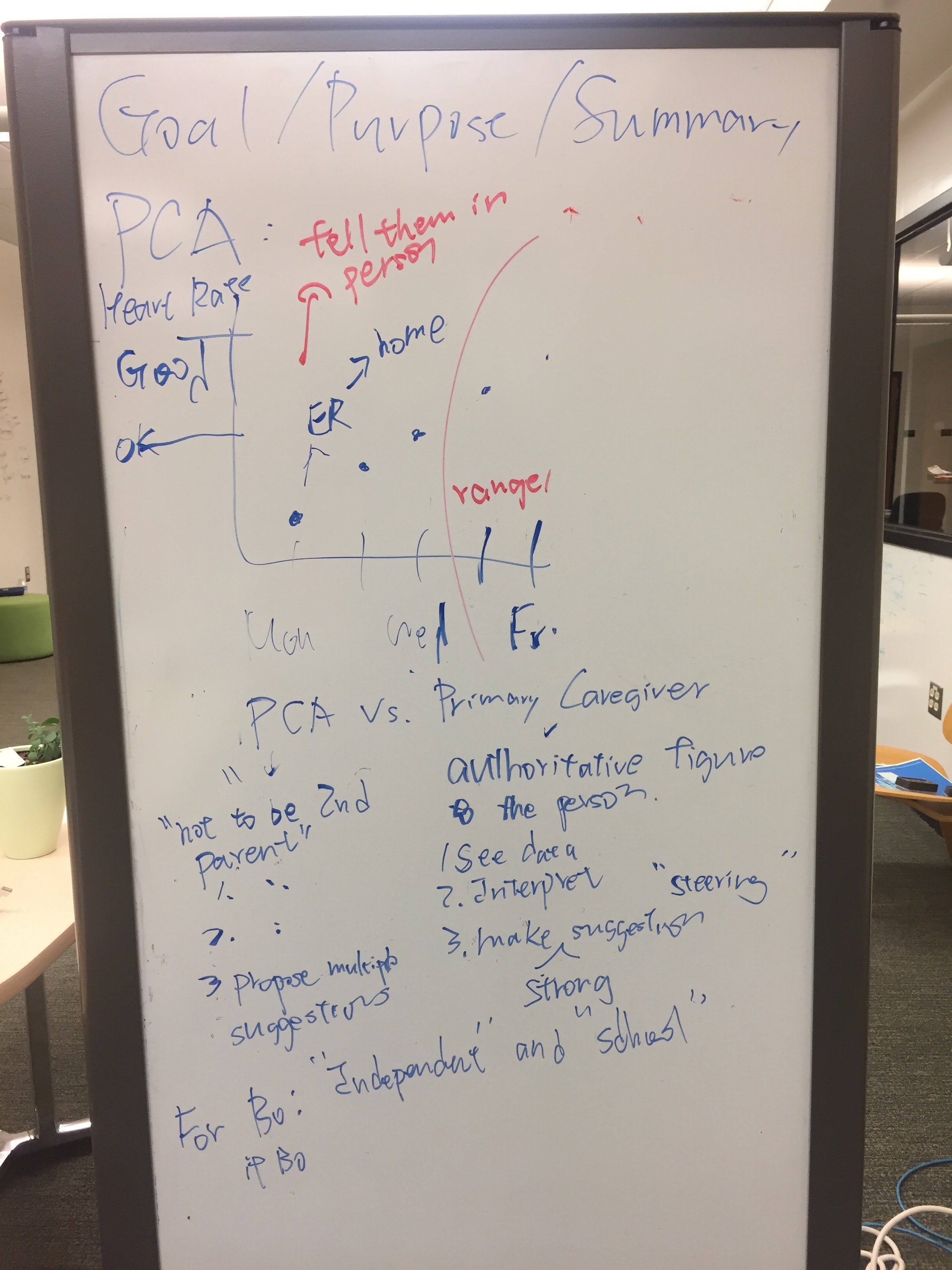
My team and I started by using semi-structured interviews and a focus group to obtain team members' experiences of managing or helping to manage the illness and care activity.
Engage Stakeholders with the Concepts of Sensors and Data through Sketches to Facilitate Brainstorming
With a solid understanding of the way care team members are collaborating and the challenges they faced currently, I then invoked sketches and other visual materials to introduce the concept of sensor and data. I employed visual materials as tools because our participants might not be familiar with the concept of sensors and data. Therefore, it might be hard for them to provide feedback simply through methods such as interviews that are heavily based on experience. The use of such visual materials helped our participants to reflect on how sensor technology could create a positive impact on their work and the unintended consequence that designers of such technology should be aware of.
Conduct Thematic Analysis to Identify Key Insights for Sensor System Design
By performing thematic analysis on the transcripts and memos, my team and I identified design implications for systems and applications that use sensor data to support care team collaboration. The two major themes were supporting routinization of care activity and allowing fine-grained control over data to share. For more details, please see the Outcomes section, including publications.
Co-Design with a Young Adult as Design Partner to Identify Key Attributes and Develop a Web System
To investigate how fine-grained control can be realistically implemented for regular users without technical training, I employed a co-design process with an undergrad student with a neurological condition for two semesters to design a mobile app for managing the sharing of sensor data. To truly engage the participant as a co-design partner, I designed a short version of the Human-Centered Design curriculum for the participant to get familiar with concepts such as persona and scenario. I invited the participant to be the designer who could bring in his own experience interacting with care team members to guide the design. Through weekly co-design sessions, I worked with the participant to design a mobile app that allowed a patient to control sensor data collected for and about the patient by regulating data sharing with care team members.
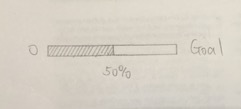
As the participant was very passionate about video games, I also explored the possibility of incorporating certain game design elements (e.g., visual) to enrich the experience for patients to understand how to control the sharing of their data, in addition to the mobile app. I have implemented a system, Data Checkers, and conducted a comparison study to evaluate the effectiveness of the design to support data sharing in chronic care.
Outcomes
Findings & Implications
Designing Technological Intervention and Support to Facilitate Routine Development
By engaging with participants through various approaches, my team and I have identified two key aspects that designers should consider. First, care activities (e.g., drinking waters and doing bowel program) are being routinized continuously for patients and care team members to provide stability of care. Sensor-based technology should tailor user engagement with different levels of proactiveness based on the stage of routinization to provide the necessary support to care teams.
Support Fine-Grained Control over Data Sharing to Balance Sharing and Privacy (Sharing Just Enough)
Second, patients desire to gain independence progressively within a complex and ever-changing care team. Patients want to control their lives but are not familiar with the nature of sensor data. Sensor-based technology should allow fine-grained control over data being shared to different care team members and provide support for patients to jump-start and understand the data sharing process. At the same time. as health, care team, and hence the care evolve, care team members will need a certain level of autonomy to access data so as to support their work effectively. Sensor-based technology should allow data sharing to be continuously negotiated among care team members.
Systems & Applications
An interactive system, Data Checkers, using a board-game metaphor such as Checkers was developed to support fine-grained control. Data Checkers' system consists of a front-end user interface and a backend server. The backend server was developed to support the interpretation and enforcement of sharing decisions. I conducted a within-subject study to compare our design with another state-of-the-art design proposed by fellow researchers. My evaluation demonstrated that Data Checkers allowed participants to effectively think and control data sharing of multiple sensor data sources with care team members and has the potential to support the long-term management of sensor data.
A mobile prototype was develooped to demonstrate the idea of allowing patients to customize how to track different data using different input controls (e.g., a text field, a slider, or a button set).
(showing the customization of mobile app? or the mobile app itself? ) https://docs.google.com/presentation/d/1SlemPpdFDhZRWyWINc17Byb-wjhPme9fkc4VPaXrTf4/edit#slide=id.g21befb6e70_0_70
(a diagram that plot the system architecture? -> but I haven't published? Maybe just some component diagram?)
(sensor table)